Blood thinners are medications that prevent dangerous blood clots that can lead to heart attacks, strokes, or deep vein thrombosis (DVT). They help maintain smooth blood flow, reducing the risk of life-threatening complications.
People with conditions like atrial fibrillation, pulmonary embolism, or clotting disorders rely on these medications. The two main types of blood thinners are anticoagulants and antiplatelets. Anticoagulants slow down the body’s clotting process, while antiplatelets prevent platelets from sticking together.
Choosing the right medication depends on factors like medical history, risk of bleeding, and doctor recommendations. Some blood thinners require routine monitoring, while others offer more convenience with fewer dietary restrictions.
Understanding the top 10 blood thinners helps patients and caregivers make informed decisions about treatment. With various options available, knowing their benefits, risks, and uses is crucial.
This article explores the top 10 blood thinners, their effectiveness, side effects, and how they work to prevent life-threatening conditions.
Types of Blood Thinners
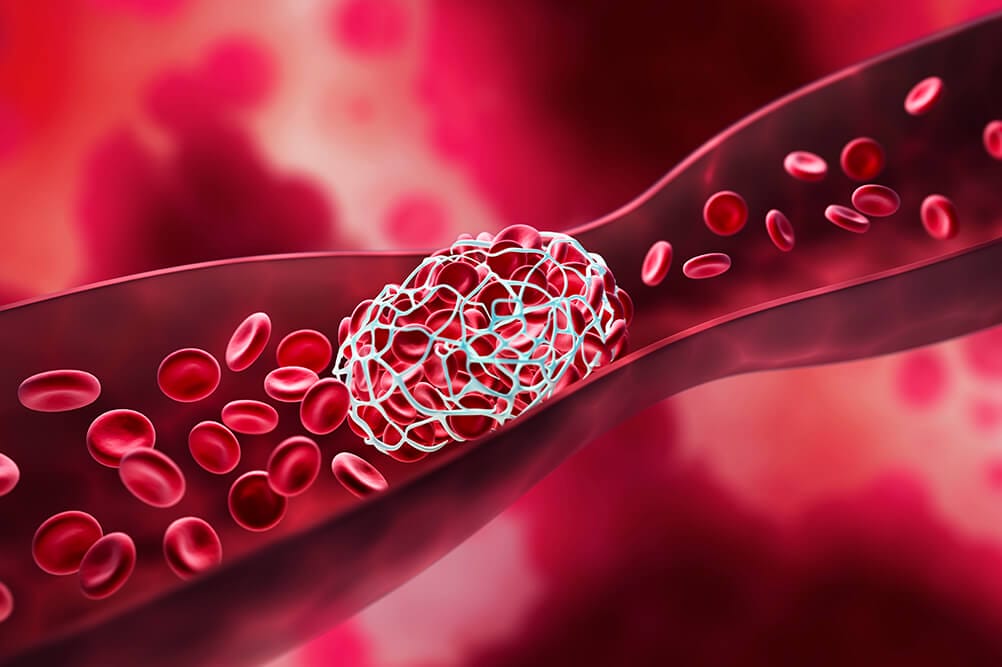
Blood thinners fall into two main categories: anticoagulants and antiplatelets. Both help prevent blood clots but work differently in the body.
Anticoagulants
It slows down the clotting process by interfering with specific proteins in the blood. They prevent existing clots from growing and reduce the risk of new clots forming.
Common anticoagulants include warfarin, heparin, and newer direct oral anticoagulants (DOACs) like rivaroxaban and apixaban. Some require regular blood tests to ensure proper dosage and safety.
Antiplatelets
It stops platelets from sticking together, reducing the chance of clot formation. They are often prescribed for people with heart disease, those who have had a stroke, or after procedures like stent placement.
Aspirin is the most well-known antiplatelet, but stronger options like clopidogrel and ticagrelor are used for high-risk patients.
Both types of blood thinners help prevent serious conditions such as heart attacks and strokes. However, they increase the risk of bleeding, requiring careful use under medical supervision.
The choice between them depends on a person’s medical condition, clotting risk, and overall health. Understanding how these medications work makes it easier to choose the right one. This article will explore the top 10 blood thinners and their specific benefits and risks.
Top 10 Blood Thinners
Blood thinners help prevent life-threatening blood clots, strokes, and heart attacks. They work by reducing the blood’s ability to form clots, ensuring proper circulation. Below are the top 10 blood thinners, categorized into anticoagulants and antiplatelets.
1. Warfarin (Coumadin)
How It Works: Warfarin blocks vitamin K, which the body needs for clot formation.
Uses: Prevents strokes, deep vein thrombosis (DVT), and pulmonary embolism (PE).
Key Considerations: Requires frequent INR blood tests to monitor dosage and effectiveness.
Risks: High bleeding risk, interactions with certain foods (leafy greens) and medications.
Warfarin has been a leading anticoagulant for decades. However, newer drugs with fewer restrictions are becoming more popular.
2. Heparin
How It Works: Enhances antithrombin, a natural clot-preventing protein.
Uses: Used in hospitals for immediate clot prevention, especially post-surgery.
Key Considerations: Administered through IV or injections, not available as an oral pill.
Risks: Requires frequent monitoring, risk of heparin-induced thrombocytopenia (HIT).
Heparin is ideal for short-term use in hospitals but is replaced by oral anticoagulants for long-term treatment.
3. Enoxaparin (Lovenox)
How It Works: A low-molecular-weight version of heparin, providing a more predictable response.
Uses: Prevents DVT, PE, and complications after surgery.
Key Considerations: Administered as a self-injection, does not require routine blood monitoring.
Risks: Can cause bruising or bleeding at the injection site.
Enoxaparin is often preferred over heparin because it offers similar benefits with fewer monitoring requirements.
4. Dabigatran (Pradaxa)
How It Works: Directly inhibits thrombin, a key clotting enzyme.
Uses: Prevents strokes in atrial fibrillation (AFib) patients and treats DVT and PE.
Key Considerations: No dietary restrictions, fewer interactions than warfarin.
Risks: Higher risk of gastrointestinal bleeding compared to some other anticoagulants.
Dabigatran is part of the newer class of direct oral anticoagulants (DOACs) that eliminate the need for frequent testing.
Read More
Top 10 Most Successful Businesses To Start In 2025
Netflix Top 10 Movies To Watch

5. Rivaroxaban (Xarelto)
How It Works: Inhibits Factor Xa, an enzyme crucial for clot formation.
Uses: Treats and prevents DVT, PE, and reduces stroke risk in AFib patients.
Key Considerations: Once-daily dosing, no need for routine blood tests.
Risks: Higher bleeding risk in certain patients, no immediate antidote for reversal.
Rivaroxaban is favored for its convenience, but caution is necessary for patients with kidney issues.
6. Apixaban (Eliquis)
How It Works: Another Factor Xa inhibitor, similar to rivaroxaban but with a lower bleeding risk.
Uses: Prevents strokes, treats DVT and PE.
Key Considerations: Preferred for elderly patients and those at higher bleeding risk.
Risks: Can still cause serious bleeding if not used properly.
Apixaban is gaining popularity because it provides strong protection against clots with fewer side effects.
7. Edoxaban (Savaysa)
How It Works: A newer Factor Xa inhibitor, working similarly to rivaroxaban and apixaban.
Uses: Prevents strokes in AFib patients and treats DVT and PE.
Key Considerations: Fewer drug interactions than warfarin, once-daily dosing.
Risks: Less effective in patients with high kidney function.
Edoxaban is a promising anticoagulant but is not recommended for all patient groups.
8. Aspirin
How It Works: Inhibits platelet function, reducing clot formation.
Uses: Prevents heart attacks and strokes in high-risk individuals.
Key Considerations: Available over-the-counter, commonly used for cardiovascular protection.
Risks: Can cause stomach ulcers and gastrointestinal bleeding.
Aspirin is the most accessible blood thinner but is less effective than prescription options for clot prevention.
9. Clopidogrel (Plavix)
How It Works: Blocks platelets from sticking together, preventing clot formation.
Uses: Given after heart attacks, strokes, or stent placements.
Key Considerations: Often combined with aspirin for stronger protection.
Risks: Some people have genetic resistance, making it less effective.
Clopidogrel is widely used, but genetic testing may be needed to confirm its effectiveness in some patients.
10. Ticagrelor (Brilinta)
How It Works: A stronger and faster-acting alternative to clopidogrel.
Uses: Prevents clotting in patients with acute coronary syndrome (ACS).
Key Considerations: More effective but requires twice-daily dosing.
Risks: Higher risk of shortness of breath and bleeding.
Ticagrelor provides powerful clot protection but must be taken with caution due to its side effects.
Risks and Side Effects of Blood Thinners
Blood thinners save lives by preventing clots, but they also come with risks. The biggest concern is bleeding complications. Since these medications slow clot formation, even minor cuts or injuries can lead to prolonged bleeding.
Common Side Effects:
Easy bruising – Even small bumps may cause noticeable bruises.
Nosebleeds – Frequent or prolonged bleeding from the nose.
Heavy menstrual bleeding – Women may experience longer or heavier periods.
Serious Risks:
Internal bleeding – Bleeding in the stomach, intestines, or brain can be life-threatening.
Blood in urine or stool – A sign of potential internal bleeding.
Hemorrhagic stroke – A rare but serious risk if bleeding occurs in the brain.
Drug Interactions:
Blood thinners interact with many medications, including NSAIDs (like ibuprofen), certain antibiotics, and herbal supplements (like ginseng or garlic). These interactions can increase bleeding risk or reduce effectiveness.
Lifestyle Adjustments:
Avoid contact sports – To prevent serious injuries.
Use a soft toothbrush and electric razor – To minimize cuts and bleeding.
Monitor diet – Warfarin users should limit vitamin K-rich foods (like spinach and kale).
Managing these risks requires careful monitoring and medical supervision. Despite their side effects, the top 10 blood thinners remain essential for preventing serious health complications.
Choosing the Right Blood Thinner
Selecting the best blood thinner depends on multiple factors, including medical history, lifestyle, and risk tolerance.
Factors to Consider:
Condition being treated – AFib, DVT, PE, or stroke prevention. Bleeding risk – Patients prone to bleeding may require a lower-risk option like apixaban. Convenience – DOACs like rivaroxaban require no routine blood tests, unlike warfarin.
Doctor’s Role:
Doctors evaluate a patient’s risk factors before prescribing a blood thinner. They consider kidney function, medication interactions, and personal preferences. Some patients need anticoagulants for life, while others use them temporarily after surgery or an acute clotting event.
A well-chosen blood thinner can prevent life-threatening conditions while minimizing complications. Understanding the top 10 blood thinners and their effects helps patients make informed decisions, ensuring safety and effectiveness in treatment.
Conclusion
Blood thinners play a vital role in preventing strokes, heart attacks, and dangerous blood clots. They help millions of people manage conditions like atrial fibrillation, deep vein thrombosis, and pulmonary embolism.
Choosing the right medication depends on several factors, including medical history, bleeding risk, and lifestyle. Some patients need routine monitoring, while newer options offer greater convenience with fewer restrictions.
Despite their benefits, blood thinners carry risks, especially excessive bleeding. Patients must follow their doctor’s instructions carefully, avoid drug interactions, and make necessary lifestyle adjustments. Regular check-ups help ensure safety and effectiveness.
Understanding the top 10 blood thinners allows patients and caregivers to make informed decisions about treatment. Whether using anticoagulants or antiplatelets, proper management is key to preventing complications. With medical supervision and the right precautions, blood thinners can significantly improve health outcomes and quality of life.